keratoconus
Depending on ethnicity, keratoconus affects up to one in 450 people. It is more common in non-caucasians. It is usually diagnosed in young people at puberty, in their late teens or early twenties.
What causes keratoconus?
The exact cause is unknown. It is believed that genetics and environmental factors play a role. It is not generally considered an inherited disease, although rarely in some families more than one individual can be affected.
How keratoconus affects vision
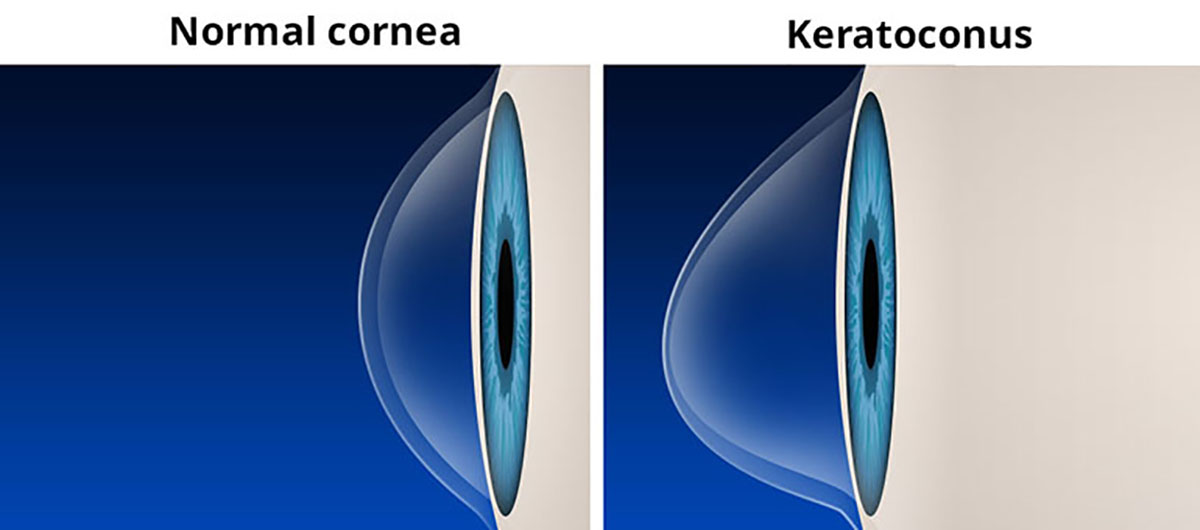
Early stages of keratoconus are detectable by your local optometrist. Vision is often unaffected in the very early stages. It is important to remember that keratoconus does not cause blindness. If left unchecked, further changes in shape, thinning of the cornea and, in advanced stages, scarring cause loss of transparency of the cornea which impairs the ability of the eye to focus properly. Even in advanced keratoconus however it is usually possible to correct vision with contact lenses.
Treatments for keratoconus
In the early stages, spectacles or soft contact lenses may be used to correct vision. As the cornea becomes thinner and steeper, soft or rigid gas permeable (RGP) contact lenses are often required to correct vision more adequately. In very advanced cases, where contact lenses fail to improve vision, a corneal transplant may be needed. This type of intervention is rare however since the introduction of corneal cross-linking (CXL). CXL is a relatively new treatment that can stop the disease getting worse. It is effective in over 94% of patients with a single 30 minute outpatient procedure.
What happens if I am referred for this condition?
Keratoconus does not require urgent referral since changes caused by the condition usually take several months or even years to develop. Because of this, we monitor those with the condition and invite them back for repeat assessments for up to five years from their initial visit.
Each time you attend this clinic, we will perform many of the same tests, including:
1. Vision (reading chart)
2. Refraction (spectacle test)
3. Corneal scans (including Pentacam)
We will compare these results with those from your previous visits. If any of the results show deterioration, we will discuss with you whether CXL is required.
CXL is only suitable where the corneal shape is continuing to deteriorate. This will be detected at your appointments. Beyond a certain stage however, if the cornea is too thin, it could be unsafe to perform the procedure. Usually in people in their late 30s, the cornea naturally stiffens and CXL is generally not required. Below this age, the cornea is more flexible and disease progression (and worsening vision) are more likely, although not certain, to occur.